Purpose Driven Research
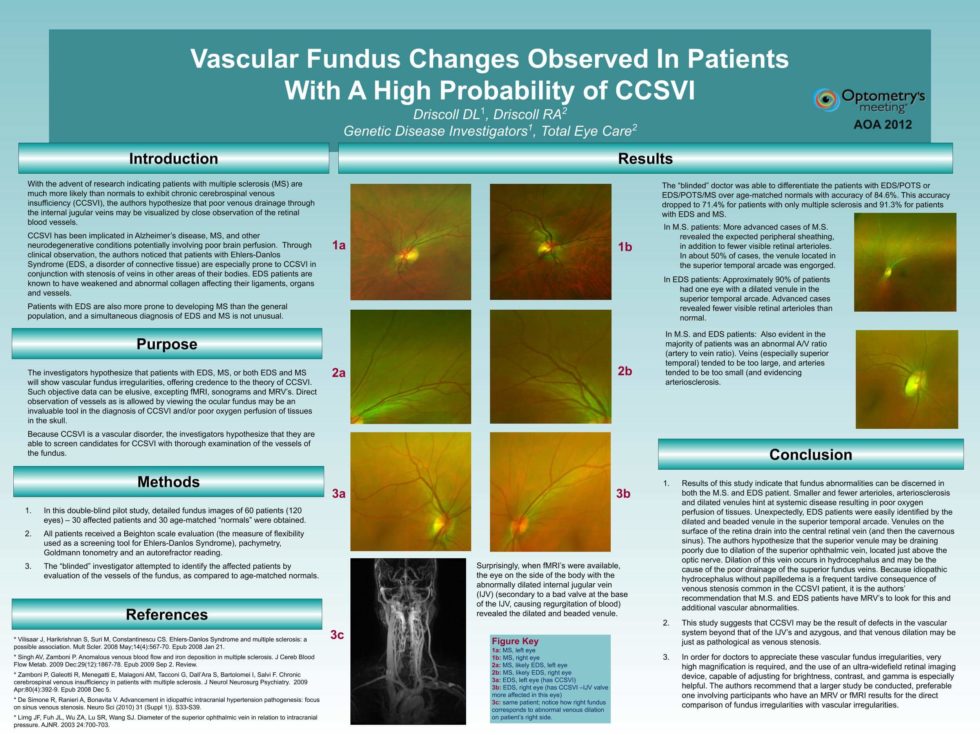
Genetic Disease Investigators LLC, Diana Driscoll, OD, President, is a global leader in autonomic research. The first to identify abnormalities of parasympathetic nerves (such as the vagus nerve), vascular problems, and intracranial pressure abnormalities, Genetic Disease Investigators LLC continues to release answers — years in advance of others.
Help us get answers! Sign up for a study today!
If you are a chronic dry eye patient interested in new treatments, we invite you to participate in these studies:
Dry Eye Survey:
Complete this 3-minute survey to see if your dry eyes could be more than just an “eye problem”.
Dry Eye Treatment Study
This exciting new study will be treating dry eyes using NeuroTears./span> This ground-breaking research uses a patented over-the-counter supplement to stimulate both inflammation control and tear production simultaneously. Please let us know if you are interested and we will reach out to you to see if you qualify.
Let us know if you’re interested!
Latest Research
The Future of Medicine Today